Publication
On optimal temozolomide scheduling for slowly growing glioblastomas
B. Segura-Collar, J. Jiménez-Sánchez, R. Gargini, M. Dragoj, J. M. Sepúlveda, M. Pesic, M. A. Ramírez, L. E. Ayala-Hernández, P.Sánchez-Gómez, V. M Pérez-García
Neuro-Oncology Advances 4(1), vdac155, 1-13 (2022)
MOLAB authors
Abstract
Background
Temozolomide (TMZ) is an oral alkylating agent active against gliomas with a favorable toxicity profile. It is part of the standard of care in the management of glioblastoma (GBM), and is commonly used in low-grade gliomas (LGG). In-silico mathematical models can potentially be used to personalize treatments and to accelerate the discovery of optimal drug delivery schemes.
Methods
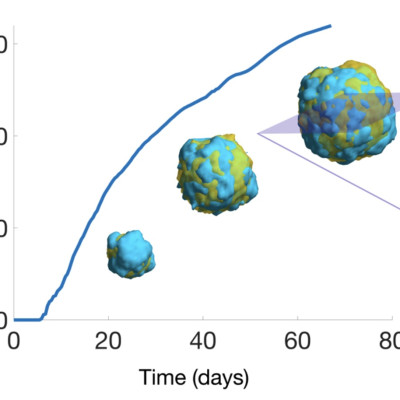
Agent-based mathematical models fed with either mouse or patient data were developed for the in-silico studies. The experimental test beds used to confirm the results were: mouse glioma models obtained by retroviral expression of EGFR-wt/EGFR-vIII in primary progenitors from p16/p19 ko mice and grown in-vitro and in-vivo in orthotopic allografts, and human GBM U251 cells immobilized in alginate microfibers. The patient data used to parametrize the model were obtained from the TCGA/TCIA databases and the TOG clinical study.
Results
Slow-growth 'virtual' murine GBMs benefited from increasing TMZ dose separation in-silico. In line with the simulation results, improved survival, reduced toxicity, lower expression of resistance factors and reduction of the tumor mesenchymal component were observed in experimental models subject to long-cycle treatment, particularly in slowly-growing tumors. Tissue analysis after long-cycle TMZ treatments revealed epigenetically-driven changes in tumor phenotype, which could explain the reduction in GBM growth speed. In-silico trials provided support for implementation methods in human patients.
Conclusions
In-silico simulations, in-vitro and in-vivo studies show that TMZ administration schedules with increased time between doses may reduce toxicity, delay the appearance of resistances and lead to survival benefits mediated by changes in the tumor phenotype in GBMs.